The CDC's Latest STI Report: Hope, Reality, and What You Need to Know
A Sex Educator's Perspective on Declining STI Rates
After a year of headlines about the rising rates of sexually transmitted infections (STIs) in the U.S., we finally have some good news to share. The Centers for Disease Control and Prevention (CDC) released its annual STI Surveillance Report, and for the first time in years, we’re seeing signs of improvement. But what does that really mean for your sexual health in 2024 and beyond?
Key Data at a Glance
The CDC’s annual report focuses on three key infections: chlamydia, gonorrhea, and syphilis (including congenital syphilis). Here’s what the latest data reveals:
Overall STI cases decreased by 1.8% from 2022 to 2023
Gonorrhea rates decreased by 7.2%
Chlamydia rates remained stable
Syphilis increased by 1% across all stages and congenital cases
Population Impact
Nearly half (48.2%) of cases affected young people aged 15-24
Gay, bisexual, and other men who have sex with men saw higher rates of STIs
Non-Hispanic Black or African Americans made up 32.4% of reported STI cases, despite representing only 12% of the U.S. population
American Indian or Alaska Native persons have the highest rates of primary and secondary syphilis and congenital syphilis
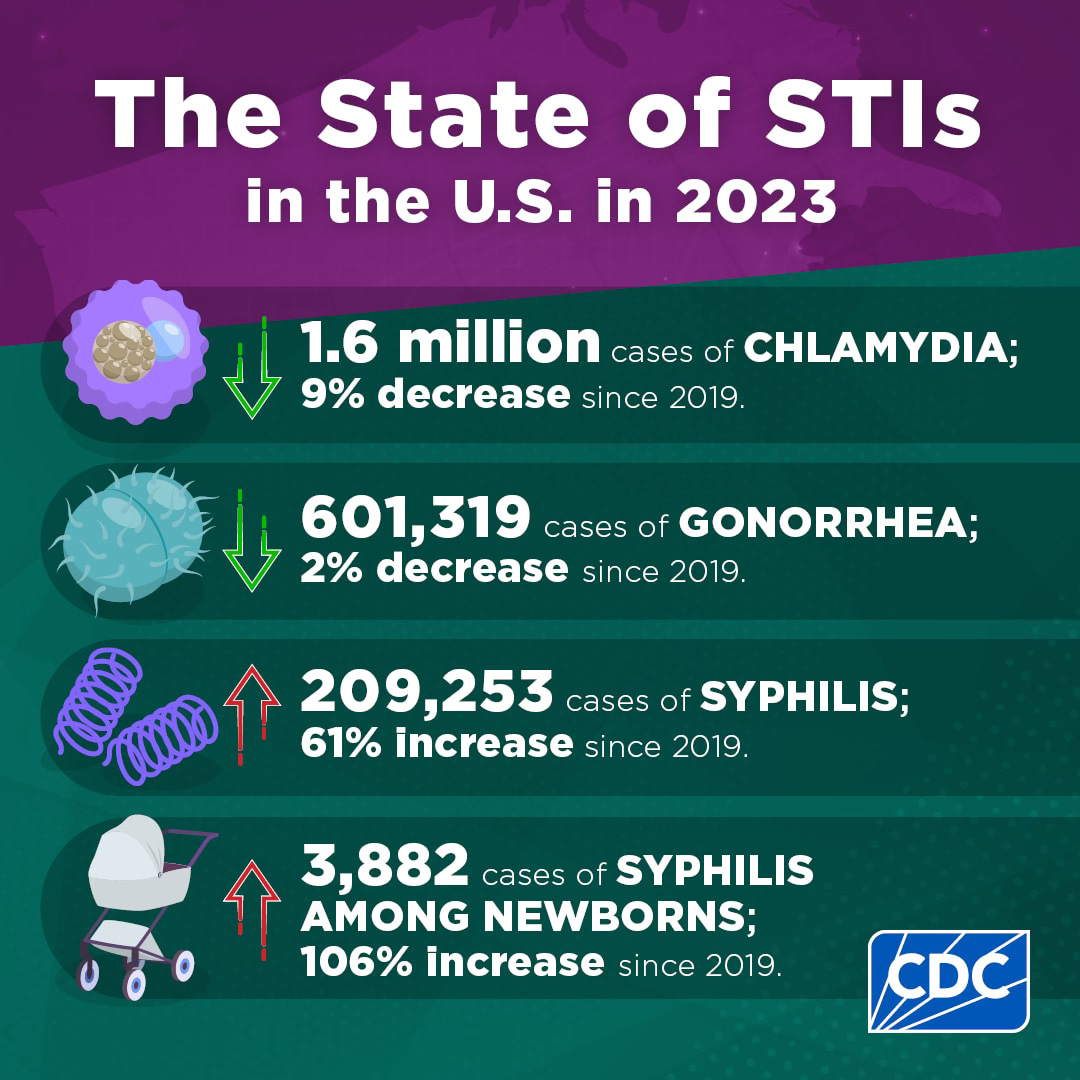
CDC (2024) The State of STIs in the U.S. in 2023
What’s Driving the Change
According to experts (including one of my faves, renowned STI specialist Dr. Ina Park!) a combination of three key factors contributed to the decrease:
increased pandemic-era funding
changes in sexual behavior among gay and bisexual men due to mpox concerns in 2022
the introduction of doxycycline as post-exposure prevention (AKA Doxy PEP)
Last month, I partnered with The National Coalition of STD Directors, who celebrated this progress, noting that "states, cities and territories were able to dramatically slow rapidly rising syphilis numbers" thanks to Congressional investment in STI prevention.
Why Aren’t All STIs Included?
If you’re wondering why some STIs aren’t included in this report, here’s why: the CDC only tracks “notifiable infections”—those that healthcare providers must legally report to public health officials. Currently, several STIs fall into this category: chlamydia, gonorrhea, syphilis, and chancroid. HIV, which can also be sexually transmitted, has its own mandated reporting system.
If you’re curious about the specifics, here’s more information about the National Notifiable Disease Surveillance System (NNDSS).
What About Herpes?
One of the most common questions I receive every year when I share my analysis of this report is, “Why isn’t herpes included?” This question often stems from stigma and an individual’s personal experience rather than public health priorities. Despite its social stigma, herpes is not considered a notifiable infection because of its high prevalence and relatively low physical health impact compared to other STIs.
A Sex Educator’s Take
As someone who brings both professional expertise in sexuality and mental health, in addition to lived experience with herpes, I want to be clear: this report is encouraging, but comes with important caveats.
First, let me clarify my role: While my work’s focus overlaps with medical and public health experts, I am neither a doctor nor a public health official. Collectively, I believe medical, public health, and sexuality professionals need to work together to shape meaningful improvements regarding STIs.
With that said, and like many experts have shared, I believe this report is an indication of good news. However, as a sex educator, I’m cautious and fearful, particularly with this incoming administration.
This report offers an analysis into three specific STIs, not STIs as a collective whole. Was there a decrease? Yes. But does this report change how we can have sex?

What these numbers don’t change:
the need for safer sex practices
the importance of regular STI testing
the ongoing conversation about sexual health
accessible STI treatment and testing for all
I’ve spent the past decade working to educate, destigmatize, and reframe sexual health as self-care, yet I still regularly encounter concerning misconceptions.
From (incorrect) assumptions like, “I don’t have any symptoms, there’s no need for me to get tested for STIs” to stigma-fueled statements like, “Don’t worry, I’m not the type of person to get herpes.” Stigma and misinformation are alive and well. Now, with reproductive rights and comprehensive sex education on the line, I fear access to medically accurate information will continue to decrease.
It's never been just an STI rate problem—we have a collective lack of comprehensive sex education problem.
Where Do We Go From Here?
While this report offers welcome news, we still face significant challenges in the battle of STIs.
Yes, the latest CDC Surveillance Report shows a decrease in STI rates—and that's worth acknowledging. But being realistic about what this means for sexually active folks isn't pessimism—it's a necessary perspective. The numbers are encouraging, but the work continues. Together, we can turn this positive momentum into lasting change.
Ready to prioritize your sexual health with honest, shame-free education? Let’s connect!
Instagram: @sexelducation
Threads: @sexelducation
TikTok: @emilydepasse
Bluesky: @sexelducation.bsky.social





