Reimagining Patient Care: Understanding the Personal Impact of a Herpes Diagnosis
In Partnership with The National Coalition of STD Directors (NCSD)
This past Sunday, October 13th, marked Herpes Awareness Day. In collaboration with NCSD, I’m sharing my diagnosis story along with professional insights on the changes I’d like to see in the future of patient care.
NCSD is a national public health membership organization representing health department STD directors, their support staff, and community-based partners across 50 states, seven large cities, and five US territories. While this piece is tailored for that audience, I believe my story and recommendations will resonate with many others as well.
As STI professionals, we often focus on statistics, education, and prevention strategies. However, understanding the personal impact of an STI diagnosis is crucial for improving our approach to both patient care and public health initiatives. This post offers insights from both personal experience and professional observation to advance our collective efforts in STI prevention, reduction, and patient support.
My Story
“This looks herpetic.”
These three words quickly shifted my mood from anxious yet hopeful to utterly terrified and disgusted in myself within a matter of seconds. I slowly closed my legs and scooted back on the examination table. I felt the tears welling. Tender, raw, violated. It may sound dramatic, but in that moment, it felt like my world was ending as I left the urgent care.
The following days were a blur of mental breakdowns and excessive drinking, all while waiting for the final phone call that would confirm my fate. Several days later, a nurse finally called. She informed me that my bloodwork was negative, but the sample came back positive for herpes simplex virus type 2, signaling a recent infection. I already felt like my fate was sealed in being alone, but my shame was further reinforced by her next comment.
“You should’ve worn a condom,” she scolded.
She couldn’t see the tears forming. She didn’t know what I had been through, or even my story or who I was outside my diagnosis. For her, testing positive for herpes said everything about who I was—or at least that’s how it felt.
When I was diagnosed with herpes in 2015, I had just graduated with honors, majoring in Gender and Sexuality Studies. My goal was to become a sex therapist, empowering women to feel confident in their bodies and sexuality. That summer, I planned to apply to graduate school and had secured a promising internship. My diagnosis shattered those plans. Suddenly, I felt not only tarnished, but also a professional failure.
Next summer marks ten years since my diagnosis. The journey to self-acceptance was slow and often painful, but it did lead me to apply and graduate from Widener University’s dual-degree sex therapy program. Herpes became a central part of my research, informing my future work and driving my passion to reduce stigma around herpes and other STIs.
Whether you’re coming from a public health, medical, or sex education or therapy background, it’s essential to recognize that each herpes diagnosis involves more than just delivering a test result. Every person diagnosed has hopes, fears, and a life beyond their infection, but the delivery of a diagnosis can quickly shift their internal perceptions and self-worth.
My experience and education have led me to identify several areas where we can improve our collective approach when it comes to herpes and STI reduction, diagnosis, and patient care.
Comprehensive Human Sexuality Training for Medical and Public Health Professionals.
Medical training is extensive, yet the average medical student receives only 3-10 hours of human sexuality training over four years. This gap in education and awareness can inadvertently lead to inadequate patient care and the perpetuation of stigma.
I often wonder if the nurse who delivered my diagnosis might have approached me differently had she received more training. In retrospect, her lack of awareness about the commonality of herpes and STIs left me feeling more shame than the diagnosis itself. While I’ll never have a definitive answer, I do know I’m not alone. Over the years, many people who have shared their herpes stories with me unfortunately expressed a similar experience of shame and judgment from medical professionals.
Partnering with sex education and mental health professionals can help bring greater understanding of the mental health impact of such diagnoses and foster a more inclusive diagnostic delivery process and support system.
Integration of Sexual Health Advocates in Clinical Settings
Health care offices and urgent care centers lack a critical component: a sexual health advocate. This person wouldn’t need to be a medical professional, but rather someone trained to understand the nuances of sexuality and its impact on mental health. Their role would be to offer nonjudgmental support and provide informed, inclusive guidance on diverse sexual identities and experiences.
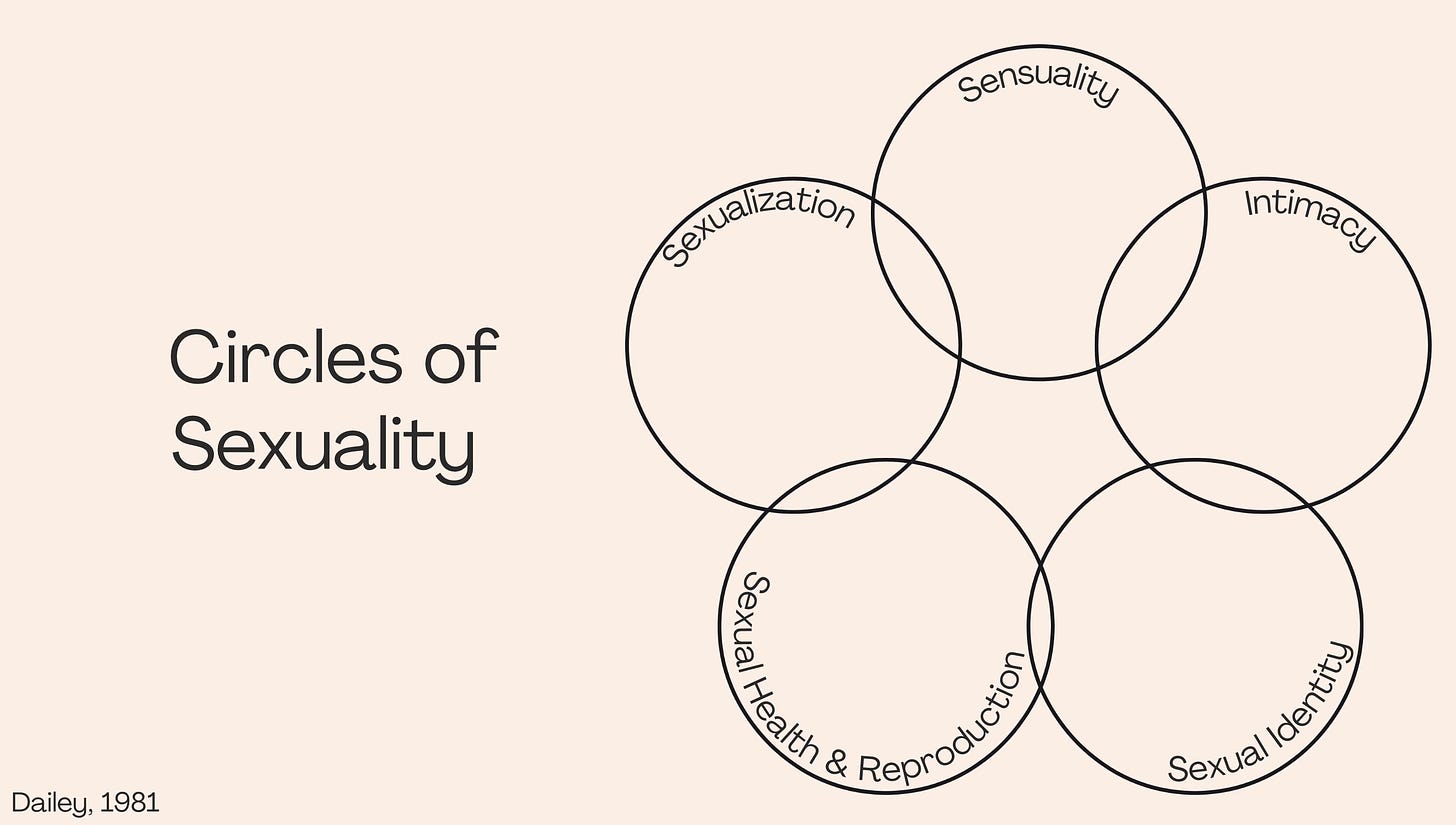
While some medical and public health professionals do seek additional education to become trauma informed and provide gender affirming care, this is not yet widespread. Moreover, many professionals focus primarily on the biological and reproductive aspects of sexual health, potentially overlooking the emotional and psychological components. This is where Dennis Daily’s, PhD, Circle of Sexuality model becomes invaluable, as it highlights five interconnected aspects:
1. Sensuality: Awareness and comfort of one’s own body; Physiological and psychological enjoyment of one’s own body and the bodies of others
2. Intimacy: The ability and need to experience emotional closeness to another human and have it returned
3. Sexual Health and Reproduction: Attitudes and behaviors related to producing children, care and maintenance of the sex and reproductive organs, and health outcomes of sexual behavior.
4. Sexual Identity: The development of a sense of who one is sexually, including a sense of gender identity.
5. Sexualization: The use of sexuality to influence, control, or manipulate others
Together, the circles are linked by values. Biases, whether conscious or not, can influence patient interactions, as seen with the nurse who delivered my results. She allowed her moral judgements to dictate her delivery—further undermining my self-worth.
A sexual health advocate who intimately understands the full scope of these dimensions could significantly improve the delivery of herpes diagnosis, particularly for underrepresented and underserved populations.
Leveraging Social Media for STI Education and Community Support
Social media has been a double-edged sword in my work—perhaps you can relate. On the one hand, platforms like Instagram have allowed me and others in sex education to share more accessible information to those who need it most. On the other, censorship and disinformation have also grown.
Many patient advocates in the herpes community use social media to bring government statistics to life by sharing personal stories, offering relatable content to people struggling with new diagnoses. However, misinformation also thrives in these spaces, often exploiting vulnerable communities, like those with herpes.
In addition to providing patients and students with traditional government websites as resources, I think it would be helpful to find reliable and informed patient advocates to include as resources for people newly diagnosed with herpes. While I spent much of my time Googling for answers about my diagnosis, many young people are turning to social media sites, like TikTok and Instagram, for not only answers, but a sense of community.
Accessible and Inclusive Language in STI Work
Accessible language is key to reducing stigma. With only 18 states mandating that students receive medically accurate sex education, many people lack even basic knowledge about their bodies and sexual health. With this framework in mind, it’s important to meet people where they are.
I’m guilty of getting caught up in theory and rhetoric that is better suited for academic audiences than the people who need it most. Accessibility in our approach is important, and does make a difference. I feel that public health, medical professionals, and sexuality professionals often share the same goal in reducing STIs and alleviating the impact of stigma, but I feel there is still a disconnect in our approach to language.
Words have their place, but they also hold power. While I am not suggesting to shift our internal field dialogues, I believe it would be helpful to the alleviation of stigma if we work together to be more mindful of language as we approach public audiences. For example, when releasing press releases about increases in STIs, new infections, or resistance to treatment, it’s almost certainly going to end up in the hands of media outlets—some reputable, others looking for clickbait. Many such outlets will employ fear-mongering headlines for public consumption, further adding to stigma, lack of testing, and reducing likelihood of seeking testing or treatment.
A Collaborative Approach to STI Reduction
While I am passionate about reproductive and sexual health, I ultimately chose sex education and therapy over medical care for two reasons: 1) I’m squeamish when it comes to bodies and blood, and more importantly, 2) my own diagnosis experience made me realize how crucial it is to have someone who truly understands the emotional and psychological impact of a herpes diagnosis.
The work clinicians and public health professionals do in disease intervention and prevention is vital, but it can’t stand alone. Sex educators and therapists help bridge the gaps left by biology and epidemiology, providing people with tools to navigate the emotional, psychological, and relational aspects of sexual health. It’s in those conversations, where stigma often lingers, that real change can begin.
Condoms, testing, and treatment are essential in STI reduction, but without the skills to have open, honest discussions about sexual health in their dating lives, people are left vulnerable. Many still don’t know how to talk about their STI status with their partners and, without those skills, prevention efforts remain incomplete. Stigma thrives in silence, and education alone won’t shift cultural attitudes unless we can also help people communicate better, too.
STI stigma, especially around herpes, has deep roots. Addressing it requires more than just medical solutions—it demands an understanding of the emotional complexities involved. By supporting people through the “awkward” and difficult conversations, and fostering more interdisciplinary collaboration, we can start to dismantle the shame surrounding these diagnoses.
It’s not about finding an immediate fix, but rather about building a culture of care where individuals feel acknowledged, supported, and empowered to navigate their sexual health without fear, shame, or stigma. The words we choose and the care we show can reshape how someone experiences their diagnosis, leaving a lasting impression on their path to healing.